PGY-6 Maternal Fetal Medicine – Western University
ResidentSenior ResidentMaternal Fetal Medicine Western University
May 2017
About Me
I’m Sheryl Choo, a resident in Maternal Fetal Medicine (MFM) at Western University. I’m in PGY-6 (deferred PGY-7 to start July 2018). I anticipate finishing in June 2019. I was born and raised in Edmonton, Alberta and started my BSc. at the University of Alberta. I was accepted to the Cumming School of Medicine before I completed the BSc. and graduated in 2011. My first residency was in Obstetrics and Gynaecology at Western University in London, Ontario. In August 2017, I’ll be starting a Master of Public Health degree in Health Policy at Harvard –School of Public Health in Boston.
The practice of obstetrics is becoming increasingly complex as the population of Canada is delaying childbearing and mothers are therefore becoming more medically complicated. That’s where Maternal Fetal Medicine plays its role. Not only do I see new pathologies and disease processes daily, I’m never bored and always learning.
I knew maternal fetal medicine was the right choice for me when I saw the depth of understanding that the subspecialists have – for example, how pregnancy changes diseases such as lupus or hypertension – and empathetically counsel patients. We work with colleagues such as pediatric surgeons for an omphalocoele, an outpouching of the anterior abdominal wall; or neurosurgery for fetal hydrocephalus and spina bifida.
At the end of the day, I’ve established numerous doctor-patient relationships with these women. We have a unique opportunity to create positive differences before babies are born, with detailed attention and preparation of an MFM subspecialist.
Clinical Life
What does a typical day of clinical duties involve?
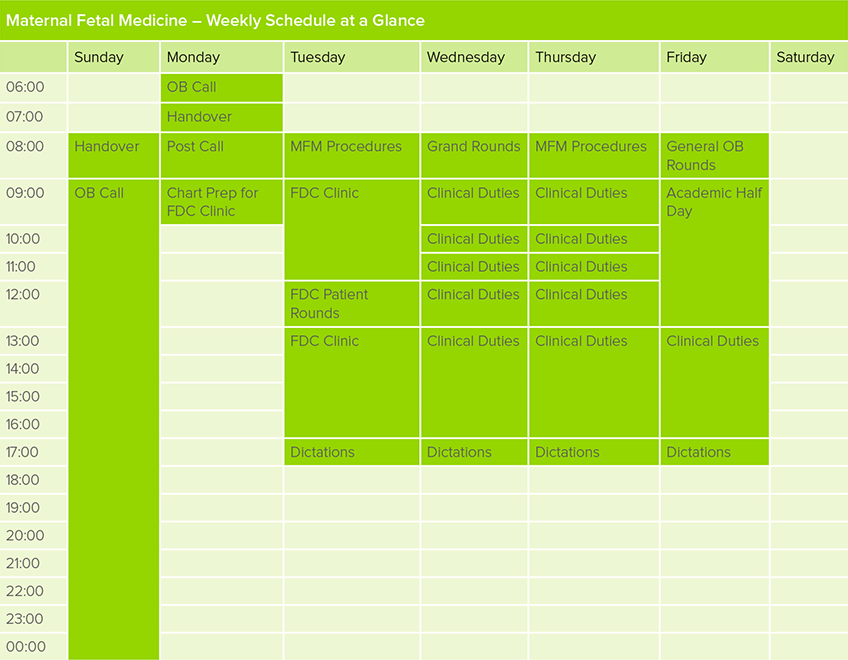
A typical day on MFM service involves procedures and clinical duties, including the Fetal Development Clinic (FDC) where we see fetuses with anomalies. On the days that FDC is not running, MFM clinics run – that is where pregnant mothers with complex diseases are seen. During OB Call days, I work with an MFM specialist and the OB/GYN resident team on labour and delivery in caring for both high- and low-risk obstetrics patients.

What kinds of clinical rotations are required in your program?
An MFM resident is required to complete rotations in the management of high-risk pregnancies in clinic and on the ward (maternal or fetal diseases), fetal ultrasound, and medical genetics. We are also encouraged to do selectives in neonatal medicine, pathology, obstetric medicine, obstetric anesthesia, fetal echocardiography. Six months of dedicated research time is embedded in the subspecialty to allow us to complete and publish projects.
Which of your personality characteristics have been particularly helpful in your field?
Maternal Fetal Medicine isn’t for the faint of heart. I think resiliency – the ability to move on from disaster to disaster – is an important characteristic in choosing MFM as a career. In the Fetal Development Clinic, we see patients who are learning about the major anomalies in their fetuses and it can be quite difficult, emotionally, as a care provider.
Empathy is critically important. Often, we are dealing with the first truly difficult life situations that these young women and families have encountered.
Finally, given that every exposure, infection and intervention needs to be assessed in the antenatal history, it is very important to be attentive to details.

What are the best aspects of your subspecialty?
Every patient presents with something unique and that keeps me captivated. Sometimes, the fetal anomalies are so complex that you really feel like a detective trying to figure what had happened, when, and how likely were the visualized changes a result of an instigating event.
Moving beyond the interesting aspects, I think that there is a distinctive difference in how MFM specialists approach their patients. In many circumstances, we are the bearer of bad news; however, we have the opportunity to embark on a distinctive relationship that may span the entire pregnancy and even into the next.
What are the most challenging aspects of your subspecialty?
Given the wealth of information that we know about maternal and fetal conditions, you would think that we have every disease down to a science or a quotable number. Unfortunately, we may never have such exact answers. The most challenging aspect of MFM is being unable to tell prospective parents exactly how an anomaly might impact their child’s future development. Nothing is more heartbreaking than telling an expectant mother that the baby they’ve been carrying may never walk, breathe, learn or interact with them after birth. Often, there’s a spectrum of what a child might be like and we can’t even give parents any numbers on impairment and development.
What is one question you’re often asked about your subspecialty?
Medical students and OB/GYN residents who are considering MFM as a future career will often ask me, “Do you ever miss gynaecology and the surgeries?” It’s a tough decision to choose a subspecialty in which you won’t be using many of the technical skills you’ve developed over the course of five years of training. Sometimes, I do miss doing laparoscopy or hysteroscopy but I know I’m so much happier and more interested in high-risk obstetrics. Not only is MFM what I want to do, my decision is easier knowing that I can contribute to obstetrics and gynaecology by being up-to-date with the newest articles and research rather than honing skills in surgery.
Can you describe the transition from clerkship into senior residency?
As an OB/GYN junior, you’re constantly learning; between assisting in gynecology ORs and managing the labour ward, it sometimes feels chaotic. Thankfully, in the senior years, there’s more time spent on subspecialties such as MFM where the pace is slower. Most residents understand that PGY-5 is an extremely trying year, given the Royal College exam and chiefing rotations and it was no different for me. I spent as much time as I could studying and made sure to take an evening once a week to spend with my family and friends.
From senior residency to MFM residency (fellowship), it’s been a fantastic change. I entered MFM because I was captivated by how diverse and challenging pregnancy and fetal medicine could be. Given that I don’t do as many OB calls, I still spend many hours during the day researching new and rare diseases.

Will you be pursuing further training or looking for employment? What resources are available to you for future-planning?
I hope that after graduation I’ll be able to find a position where I can continue to care for high-risk obstetric patients while taking a larger role in health care leadership. In particular, I hope to be involved at my local hospital to create health policies geared towards patient care and economic efficacy as well as at a national level with the Society of Obstetrics and Gynaecology, where many of the standard-of-care guidelines are created.
Non-Clinical Life
What are your academic interests (e.g. leadership activities, research)?
During my OB/GYN residency at Western, I was elected as Resident Training Program representative for two years and had the opportunity to be part of the Society of Obstetricians and Gynaecologists Junior Member Committee. Through networking with OB/GYN residents across Canada and the issues affecting trainees, staff, and patients, I knew I wanted to be more engaged in health policy.
Beginning in August 2017, I’ll be heading to Boston to complete a Master of Public Health in Health Policy. I hope to return to Canada with the tools to not only create health policies in maternal fetal medicine but to also have the skills to understand how to evaluate the effects, efficacy, and cost-effectiveness of our interventions.
What is your work-life balance like, and how do you achieve this?
I’m very close with my residency peers, particularly with the group in my year. We have a group chat where we talk about difficult cases, new evidence, and just everyday life. They are a great source of support and stability in residency. The other reason why my group gets along so well is our mutual love of board games. Twice a week, we get together to play games like Eclipse, Seafall, or 7 Wonders.
All fun and games aside, I make sure to set aside time for myself each day. I may head to the gym or spend an hour reading a novel – things to keep my mental health well. The other parts of my life that keep me grounded are my partner and my little terrier, Apollo. It never hurts to head to the dog park and watch a dozen puppies play



