PGY-4 General Internal Medicine – University of Saskatchewan
FellowInternal Medicine University of Saskatchewan
October 2018
About Me
I’m Jonathan Dean, a fourth-year, general internal medicine fellow at the University of Saskatchewan. I received my medical degree through the University of Saskatchewan in 2014 and had previously completed a bachelor’s degree in biochemistry at the University of Regina. I am from Regina, Saskatchewan.
Why I chose general internal medicine
As a medical student, I felt inspired by general internal medicine (GIM) physicians. Not only were they able to work through both acute and chronic complex medical problems, but they were advocates and coordinators for the care their patients needed. I felt subspecialty rotations less rewarding when the consulting team was more narrowly focused around one or two of a patient’s issues.
In residency, I became increasingly interested in medical education and leadership. The breadth of general internal medicine provided an excellent opportunity to teach and supervise medical learners. Indeed, the culture of general internal medicine encourages physicians to engage in medical education, leadership, quality improvement, or other areas of interest. A general internal medicine subspecialty fellowship gave me the opportunity to start a Master’s in Medical Education, which I plan to overlap with my fifth year of fellowship.
Clinical Life
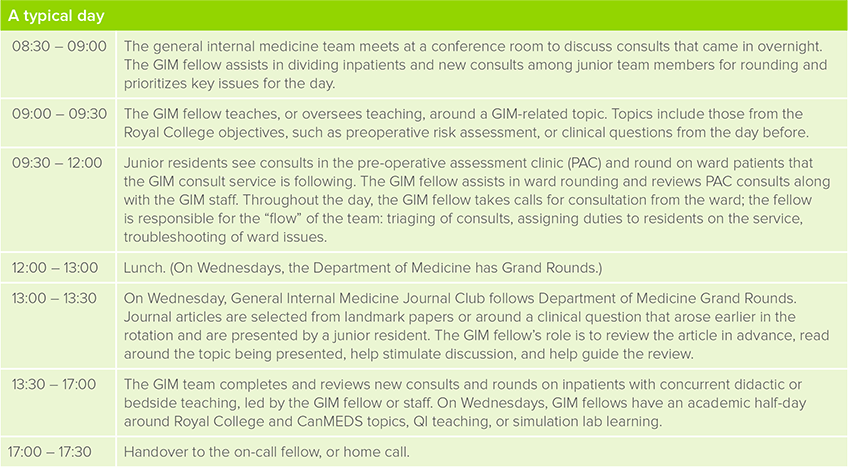
What does a typical day of clinical duties involve?

What kinds of rotations are required in your program?
The GIM specialty program has many elective opportunities (more than six months over two years), allowing a fellow to find an area of interest or pursue training relevant to their eventual place of work. In my case, I will be working on additional training in medical education. Fellows are provided with both tertiary and community hospital experiences that include time at a tertiary hospital on CTU or GIM ward consultation services, at community hospitals as junior attending in either the emergency room or on an inpatient service, and at a rural community hospital for one month or more.
Additional experiences include critical care, obstetrical internal medicine, pre-operative assessment clinics, electrodiagnostics clinics, and outpatient GIM and specialty clinics. Every GIM fellow in our program has a longitudinal clinic, where we see our own assigned outpatients, follow up on labs, arrange follow-up, and direct care as needed under the supervision of one or two general internal medicine consultants.
Which of your personality characteristics are particularly helpful in your field?
An interest in working with other people is very helpful. General internists are surrounded by a clinical team that includes consultants, nurses, allied health care providers, patients, and patients’ families. Communication with each of these team members is essential to getting someone the right care at the right time and understanding a patient’s goals of care in the first place. Also, while an interest in teaching is not essential, I have found it an asset. Medical learners work on general medicine services throughout their training and depend on staff general internists for advice and supervision.
What are the best aspects of your residency?
The culture of GIM supports pursuits outside of clinical medicine, such as medical education, leadership, and quality improvement. The GIM specialty program enables fellows to pursue not only their clinical aspirations, but also those that will complement their clinical work. In addition, general internists work closely with multidisciplinary teams that attend to the entirety of a patient’s needs. The GIM specialty program provides learning opportunities in junior attending and oversight roles meant to expose fellows to this coordination of care, both in inpatient and outpatient settings (i.e. longitudinal fellow’s clinic).
What are the most challenging aspects of your current role?
One of the challenges of GIM is defining one’s scope. As a general cardiologist, for instance, you would not see a patient for management of chronic kidney disease. The GIM specialist is trained to manage most internal medicine presentations without assistance for 24 hours. GIM physicians also receive dedicated training in obstetrical medicine and pre-operative risk assessment. As such, it is not easy to predict what consults or admissions a general internal medicine physician will look after. General internists need to be comfortable with this degree of unpredictability. Furthermore, given the variety of care GIM specialists provide, they need to know a spectrum of clinical guidelines and keep up to date with changes in practice.
What is one question you’re often asked about your decision to pursue a non-clinical career?
In addition to questions about scope, residents often ask what is “gained” by specializing an extra year in GIM, rather than graduating after four core years as an internal medicine physician. The GIM subspecialty program provides additional experiences in obstetrical medicine, perioperative medicine, electrodiagnostics, critical care, and longitudinal and outpatient care. There is extra focus, at academic half-days, on non-medical expert topics, such as quality improvement. Further, the extra year allows a fellow to round out their training with additional electives in areas of interest or need.
Describe the transition from junior resident to senior fellow.
I did not move to a new city for subspecialty training, so I did not experience the pressures that go along with finding a new place to live. My transition to fellowship was more about taking greater ownership of clinical decision making, gaining comfort with applying medical knowledge in outpatient settings, and learning to coordinate a team of medical learners.
As a junior resident, the relationship between you and your staff feels more like close supervision; a good portion of your medical decisions are run by the more senior resident or staff doctor. As a fellow, the fellow-staff relationship evolves into mentorship. There’s trust that you know the basic principles of medicine, and your plan more often directly affects clinical care. To adapt, I found that I was taking more time to check my decisions, read around patients, and brush up on guidelines. This was also my experience in outpatient settings and when giving phone advice on call. On the flip side, it is immensely rewarding to know that you have had a more direct, meaningful, and beneficial impact on a patient’s clinical course.
Overseeing a team of medical learners presented its own challenges. As a fellow, you take on more responsibility for ensuring patient safety. You also take a larger role in driving the teaching and the growth of learners under your supervision. Part of the learning curve in fellowship is being able to identify your team’s strengths and weaknesses. This directs how you spend your time teaching and how you spend time seeing patients on the ward. GIM staff are very open to discussing their own concerns and thoughts around learning needs; these open discussions helped me to shift into this new role.
Describe your experience with the subspecialty matching process. What resources did you find helpful for this?
I ensured that I had done GIM electives in each of the programs I was most keen to apply for. Even if my preferred rotation (ER consults) was unavailable at a site, I would choose another GIM rotation there (e.g. ward consults). I did not do electives outside of GIM until fellowship; I wanted to ensure that each program had met me and that I had a reference letter from one or two GIM staff at each institution. I found the process of writing personal letters took longer and was more difficult; you are not only thinking about the resources and unique training opportunities in each location, but you are also thinking about how matching to each program may affect your scope or location of work after licensure. I would highly recommend seeking out program directors and fellows in programs of interest to ask them about their clinical and non-clinical experiences.
Will you be pursuing further training or looking for employment? What resources are available to you for future planning?
I plan to start a Master’s in Medical Education concurrently with my fifth year of GIM training. I will finish this program in my second year of practice.
Our program circulates job opportunities. Our program director is happy to provide career advice or help to find specific resources. There is a curriculum around transition to practice embedded in our fellowship program.
Non-Clinical Life
What are your academic interests?
My interests are in related areas of medical education, leadership, and wellness. For example, I am working on a research project to examine residents’ perceptions of clinical feedback. I serve as resident representative to the Competency by Design Implementation Working Group, which is the local post graduate medical education committee that oversees integration of competency-based medical education into Royal College programs. I have an active role as past-president and GIM representative to the board of Resident Doctors of Saskatchewan, and am past co-chair of Resident Doctors of Canada’s wellness committee. I have given presentations on feedback, intimidation and harassment, and burnout.
What is your work-life balance like, and how do you achieve this?
Achieving a work-life balance for me might look a little strange because I find it enjoyable to go from clinical duties to a leadership commitment and back. However, I feel that true, protected non-medical time is a necessary part of staying well. Vacation time should be spent on vacation away from work, and conference leave should also involve enjoying the city you’ve traveled to.
When not studying for Royal College, I play water polo weekly with a community-based group and dabble in occasional pick-up volleyball and jogging. My wife is training our golden retriever as a search and rescue canine; hiding in the forest to be found by a tail-wagging golden retriever is an incredible stress-reliever.
You can find Jonathan on Twitter @drjondean



