PGY-5 General Endocrinology – University of Ottawa
ResidentSenior ResidentEndocrinology University of Ottawa
July 2017
About Me
My name is Jill Trinacty, and I was raised in Berwick, Nova Scotia. I went completed my BSc. (Honours) at Saint Francis Xavier University in Antigonish, Nova Scotia. I spent a year as the Active Living Coordinator with the Town of Kentville then completed my MD at Dalhousie University. I moved to Ottawa, Ontario in 2013 for my residency in Internal Medicine at the University of Ottawa and am currently a PGY-5 in Endocrinology and Metabolism.
In medical school I became interested in almost every area of medicine, but ultimately applied to internal medicine for a number of reasons. I have always been interested in Endocrinology, specifically diabetes. Diabetes affects so many people in our communities and can have significant morbidity and mortality. I liked the detail of internal medicine and the complexity of patients. Having some previous experience in public health, I knew that I wanted a career that would allow me to discuss lifestyle changes as an aspect of therapy – specifically nutrition and physical activity. I also wanted a career that would allow for work/life balance. Seeing the day-to-day lifestyle of each internal medicine subspecialty confirmed that Endocrinology was the right fit for me.
Clinical Life
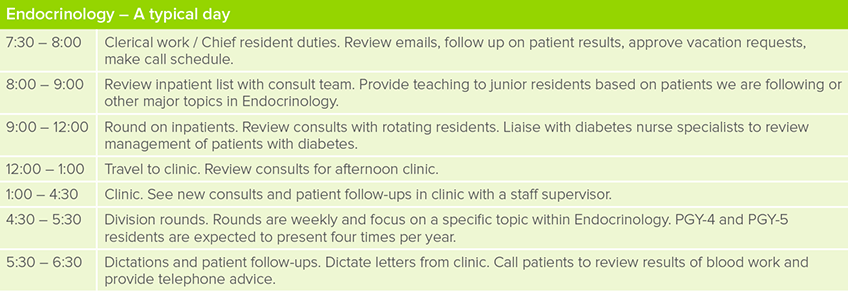
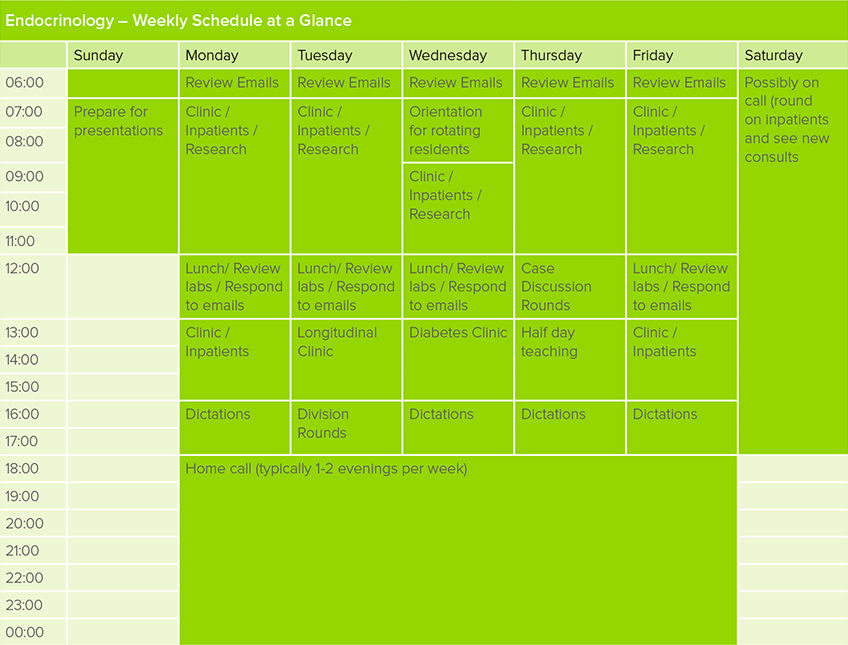
What does a typical day of clinical duties involve?
This is an example of my typical daily and weekly schedule:
What kinds of clinical rotations are required in your program?
The PGY-4 year of Endocrinology involves clinic-based blocks and inpatient consultation service. Subspecialty rotations include bariatrics, women’s health, reproduction, lab biochemistry, nuclear medicine, and pediatrics.
The PGY-5 year is more tailored to your interests and can be research-focused, with up to four blocks for research. Community Endocrinology can be done in the 4th and 5th year. There is also opportunity for elective blocks at other institutions.
Which of your personality characteristics have been particularly helpful in your field?
Being organized and self-disciplined is an asset in any specialty, because being prepared when you see a patient helps to establish trust and develop the therapeutic relationship, which can sometimes be difficult as a learner. Reviewing test results before patients come to clinic and knowing what the next steps will be shows that you care and are working with the patient to improve their health.
What are the best aspects of your residency?
Seeing improvement in patients’ conditions and working as a team to support patients. It is so rewarding to have a patient achieve results with lifestyle change, and to follow the same patients over time and adjust management of their conditions based on their particular needs.

What are the most challenging aspects of your residency?
The most challenging aspects of this specialty are patient engagement and keeping track of lab work and outpatient testing. Diabetes requires consistent day-to-day effort and sometimes patients have a lot on their plate. Diabetes may be the last thing they think about. It’s important to keep that in mind when seeing a patient, because although diabetes is the number-one focus for you during the clinic visit, it may not be for them.
This specialty also involves a lot of outpatient lab testing and imaging that needs to be reviewed between visits. Keeping track of this as a resident can sometimes be difficult.
What is one question you’re often asked about your residency?
“Is it all diabetes?”
Many medical students, residents, and even other clinicians often perceive Endocrinology to be all about diabetes management. That is about 50% of what we see in clinic. We are also often managing a variety of thyroid issues, parathyroid, bone metabolism, adrenal and pituitary disease. Many of these clinical issues can be definitively managed, and treatment often results in a significant improvement in the patient’s well-being, which is very rewarding as a clinician.

Can you describe the transition from clerkship into residency?
The transition from junior resident to senior resident in core internal medicine comes with a focus on the role of the physician as manager. Transition from core internal medicine to subspecialty resident was a bit more difficult to navigate because you take on more of a supervisory role and need to let junior residents have autonomy while providing teaching and support.
Will you be pursuing further training or looking for employment? What resources are available to you for future-planning?
After I complete my PGY-5 year, I will pursue employment. After a decade of training I am ready to work! Future planning is mostly done on your own. Often, institutions will contact the program director with information about open positions and it is up to the trainee to pursue it if it is of interest. For those looking for a career in academic medicine, it is typically expected that the trainee will pursue a Master’s or PhD in a clinical scholar position. In this position, you act as staff with your own clinics and you have protected time to pursue your studies.
Non-Clinical Life
What is your work-life balance like, and how do you achieve this?
Work-life balance was a bit difficult in PGY-4, as the year is heavily focused on studying for the internal medicine Royal College examination. I was fortunate to have a very supportive group to study with who made the process much easier.
Personally, I engage in physical activity as a way to manage stress and find it helps to clear my mind. I am also a big planner, so I try to map out my week, month, and year so I can allot time to work on projects, presentations, and so on without feeling too rushed or stressed. It is also important to schedule in vacation time and relaxation time and to take full mental breaks from work.
You can follow Jill on Twitter @jtrinacty



