PGY-5 Psychiatry – McMaster University
ResidentSenior ResidentPsychiatry McMaster University
December 2015
About Me
I’m Natasha Snelgrove, a PGY-5 in psychiatry at McMaster University in Hamilton, Ontario. I graduated from the University of Alberta medical school in the Class of 2011.
I’ve always been interested in psychology and the brain, even when I was doing an undergrad degree in psychiatry. If I hadn’t gotten into medical school, I was planning to apply for a PhD in psychology. I found mental health issues very interesting to deal with and treat. The fact that psychiatry is a lot younger than other disciplines in terms of research and treatments was very appealing to me. I also really liked the aspect of psychiatry that lets one get to know patients really well and treat them over a period of time during their lives.
Clinical Life
What does a typical day of clinical duties involve?
In psychiatry, residents work closely with one or two staff preceptors. We tend to have maximum interaction with them and less interaction with fellow residents, who are all rotating on different units/clinics and with different staff.
Usually I’m either on an inpatient or outpatient rotation, which look a little different. On inpatient rotation, I have particularly close interaction with nursing and social work staff, as they’re usually key to my patient’s eventual treatment and discharge plan. We have weekly team rounds with all the interprofessional staff. On outpatient rotation I work more closely with nursing or social work clinicians, who typically provide patients with therapy, and sometimes with family physicians, depending on the clinic set-up. There also are interprofessional team meetings, but they are a little less frequent.
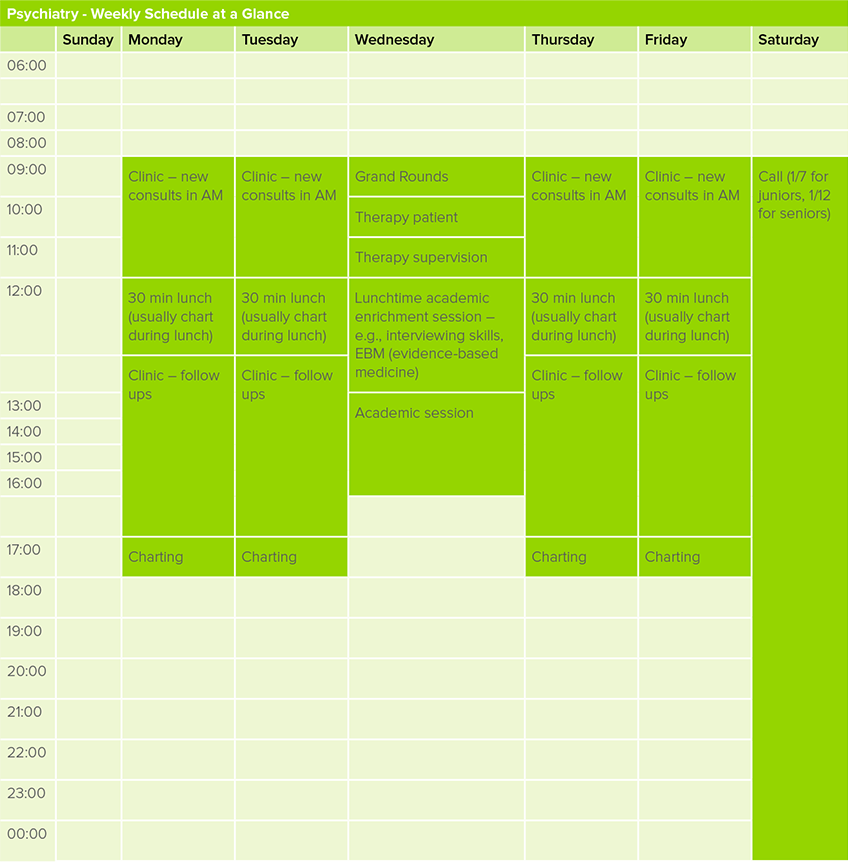
Teaching happens on Wednesdays, which is a full academic day. Usually this means Grand Rounds first thing in the morning, followed by longitudinal therapy patients (we have to carry five longitudinal patients sequentially during residency for CBT [cognitive behavioural therapy] and other kinds of therapy) and therapy supervision, with didactic or small group teaching in the afternoon.
Call for junior residents is 1 in 7 and for seniors it is 1 in 12. We do call exclusively for emergency (e.g., seeing consults) and do not manage ward issues.
What kinds of clinical rotations are required in your program?
In PGY-1 residents complete two blocks of internal medicine and one block of all other rotations – pediatric neurology, adult neurology, emergency psychiatry, neuroradiology, family medicine, addictions, and emergency medicine – plus two selective blocks (peds, palliative, and geriatrics are common choices), and one elective block (usually done in an area of psychiatry).
In PGY-2 and PGY-3, all core clinical rotations are done – six months inpatients, six months outpatients in PGY-2; six months child (inpatients and outpatient components) and six months geriatrics (inpatient and outpatient components) in PGY-3.
PGY-4 includes six months of rehab/chronic care (severe mood disorders or schizophrenia are common rotations), three months of consult liaison (consulting to medical floors for psychiatric issues), and three months of collaborative care (usually working directly with family doctors in a Family Health Team setting).
PGY-5 is all selectives and electives, so one has a lot of freedom to pick areas of personal interest (e.g., child, geriatrics, mood disorders, schizophrenia, general outpatients). For those who want to pursue either a child or geriatrics fellowship, this year can be double-counted towards that fellowship (both of which are two years and entail a PGY-6 year).
In addition to clinical rotations, we’re required to complete five modules of longitudinal psychotherapy with patients, including emotion-focused therapy, CBT, psychodynamic therapy, and interpersonal therapy. We typically see these patients on Wednesdays or at the end of a clinical day in order to fit them into the busy schedule.
Which of your personality characteristics have been particularly helpful in your field?
Empathy and communication skills have been the most helpful in working with psychiatric patients, their families, and their care teams. Psychiatry is typically a very collaborative specialty, so the ability to work well with teams has been key.
What are the best aspects of your residency?
I love the patients I work with and the collaboration with interprofessional team members and family physicians. It is also really nice to have longer term relationships with patients on many rotations, to see them get better over time, and know how much they appreciate our care.
What are the most challenging aspects of your residency?
Sometimes psychiatric patients and, at times, their families can be very challenging to work with due to the nature
of their illnesses. In addition, tension within teams can also run high; there can be problems and communication breakdowns among interprofessional staff, especially in high-stress settings like the emergency room. Since we have longitudinal aspects to our residency (carrying therapy patients), it is sometimes challenging to fit their time in around busy clinical rotations. Staff are not always the most understanding when we have to leave a clinical rotation to go do a different kind of work. Sometimes they pressure us to stay, as if we’re not actually responsible for seeing another patient who needs our care.
What is one question you’re often asked about your residency?
“Psychiatry? Why would you ever want to do that?” I think a lot of people misunderstand psychiatry as being all about really difficult patients and families. Like any specialty, we have those cases, but we have a lot of patients who are really interesting. It’s very satisfying to help them get better and get back to work and their lives.
Can you describe the transition from clerkship into residency?
Scary! The first time you’re the one signing orders, you recheck your dosing several times! However, I found I was well supported by senior residents and my staff, so it was a rather smooth transition. It was probably helpful that I started on peds neurology and not on internal medicine; that transition was really smooth, with all the staff and residents being really helpful and understanding, but also giving me independence as I was ready for it.

What are your future practice plans?
I plan to practice general outpatient psychiatry. I have an interest in adolescent/young adult mental health, given that there is so much one can do in terms of primary and secondary prevention in these age groups. I’ll probably work in a
Student Health Centre on a university campus. There is a lot of need for psychiatrists, so finding a position usually isn’t too much trouble as long as one has connections and is willing to explore options and take interviews.
What are your fellow residents like and how do you interact with each other?
Overall, my fellow residents at Mac are pretty great – most of us are collegial and support each other well. We do a few social events a year as well, like a resident Christmas party, which keep us connected.
Because in psychiatry we often are working more independently with staff instead of with fellow residents, we keep connected by seeing each other on academic days, being on call together (we have a junior-senior paired model), and going to social events.
Non-Clinical Life
What are your academic interests (e.g. leadership activities, research)?
I’ve been really active in leadership, particularly since PGY-2. I am currently the president of the Professional Association of Residents of Ontario (PARO) and a board member and co-chair of the training committee at RDoC.
I also explored doing research in PGY-3 through some longitudinal research time my program provided to me. Ultimately I found the pace of research too slow and decided against pursuing a career track in that direction.
I’ve been very fortunate that my program has supported me through this, even more so in my upper years as my leadership load has gotten bigger. I think they see it as both an asset to my professional development and to the department, especially since I’ve always been very conscientious to meet my professional responsibilities at work and in my program.
When I have finished my program, I plan to pursue an academic career, probably focusing on teaching and local quality improvement initiatives.

What is your work-life balance like, and how do you achieve this?
My work-life balance could be excellent – and many other residents in my program do experience this and take full advantage – but given my strong interest in leadership opportunities, mine is not!
As I’m quite involved locally, provincially, and nationally, I’m often at meetings on the weekends and don’t have a lot of time for myself.
However, I really do prioritize my physical fitness. I run and do yoga regularly, despite my schedule. Those things keep me sane!
Other residents in my program who are less involved in extracurricular interests often have very interesting hobbies.
Since our call schedule is very reasonable – as is the typical workday (8–9 am until 5–6 pm) – this leaves time for activities outside residency.
Many residents also choose to start their families in residency. I think Mac Psychiatry must be the most fertile program at McMaster! The program is really supportive of residents taking maternity or paternity leave and balancing those responsibilities on their return.



